With concerns mounting over the possibility of an Ebola outbreak expanding beyond West Africa, government and health officials are re-evaluating protocols and procedures — and at the same time, looking to quell public fear.
Gov. Andrew Cuomo yesterday convened a news conference to outline the New York’s plans for Ebola preparedness and assure residents that the state is “taking every precaution to protect their health and safety.”
Cuomo designated eight hospitals statewide to treat Ebola patients, including Stony Brook University Hospital and North Shore/LIJ on Long Island.
The state health commissioner yesterday issued an order to all hospitals, diagnostic and treatment centers, and ambulance services in New York State, requiring that they follow protocols for the identification, isolation and medical evaluation of patients requiring care.
Changing protocols and guidance from CDC
Local hospital administrators, who have been processing new directives and guidance documents from the Centers for Disease Control on an almost daily basis for the past week or so, are working to sort out how protocols and procedures are changing, PBMC Health president and CEO Andrew Mitchell said last night.
 “It’s clear that the Ebola situation and guidance from CDC is extremely fluid and being constantly updated,” Mitchell said. “That began with the changes they made in the last week on personal protective equipment for heath care workers and a new recognition that it is better to treat patients in highly specialized regional facilities than to care for them in every hospital,” he said.
“It’s clear that the Ebola situation and guidance from CDC is extremely fluid and being constantly updated,” Mitchell said. “That began with the changes they made in the last week on personal protective equipment for heath care workers and a new recognition that it is better to treat patients in highly specialized regional facilities than to care for them in every hospital,” he said.
“What that translates into is that every hospital, including PBMC, needs to initally be able to diagnose an Ebola patient and then work with specialized treatment facilities to arrange the safe transfer of such patients,” Mitchell said.
The current protocols spell out the type of personal protective equipment that should be worn by all health care workers coming into contact with a patient who has both symptoms of infection and specific risk factors within the past 21 days before the onset of symptoms.
Symptoms include fever of greater than 101.5 degrees Fahrenheit, and additional symptoms such as severe headache, muscle pain, vomiting, diarrhea, abdominal pain, or unexplained hemorrhage.
Risk factors within the past 21 days before symptom onset include direct contact with blood or other body fluids or human remains of a patient known to have or suspected to have Ebola Virus Disease; residence in — or travel to — an area where EVD transmission is active; or direct handling of bats or non-human primates from disease-endemic areas.
The protocols also detail procedures for EMS systems and public safety dispatchers for identifying and managing patients with known or suspected EVD, and screening procedures in communities where the risk of Ebola is considered elevated — communities where patients with confirmed Ebola are identified in the area.
Cuomo also announced coordination by the Port Authority of procedure and practice between all airports to ensure proper training is in place.
Congressman alarmed by in-flight death on Nigerian flight to JFK
 But yesterday, Rep. Peter King (R-Seaford), chairman of the House subcommittee on Homeland Security, wrote to the secretary of the U.S. Dept. of Homeland Security demanding answers regarding the handling of airline passengers from countries affected by the Ebola outbreak. Read King’s letter here.
But yesterday, Rep. Peter King (R-Seaford), chairman of the House subcommittee on Homeland Security, wrote to the secretary of the U.S. Dept. of Homeland Security demanding answers regarding the handling of airline passengers from countries affected by the Ebola outbreak. Read King’s letter here.
King was alarmed by the in-flight death of a passenger on a flight from Nigeria to JFK yesterday. The passenger reportedly died after vomiting aboard the plane. King said in the letter he has “very serious concerns” about the handling of the passenger’s remains and the “cursory exam” conducted by a CDC official at JFK before declaring that the passenger did not have Ebola. He said the CDC failed to give adequate instructions to Customs and Border Patrol and Port Authority officers regarding handling the deceased passenger’s remains or the rest of the passengers on the plane.
King said 70 to 100 passengers from countries impacted by Ebola arrive at JFK daily — two-thirds of all passengers of concern entering the U.S. every day.
“These individuals transit the airport with the rest of the traveling population, including using the restrooms,” King wrote. They are segregated from other travelers only after they arrive at the Customs and Border Protection office, he said.
“Given the high volume of travelers at JFK, it is essential that extraordinary measures are taken to intercept possible Ebola-infected passengers while keeping the public, CBPOs [Customs and Border Protection Officers] and other first responders safe from exposure,” King wrote.
King demanded answers from the homeland security chief by today.
PBMC chief: Hospital screening systems will be quickly overwhelmed
 With Ebola transmissions now documented in the U.S. and Europe — something that never happened before the current Ebola outbreak in Africa, which is the most widespread since the disease was first identified there in the 1976 — health officials worry about “loss of containment.” That worry is not just a concern about the spread of the disease itself, but also for the impact loss of containment will have on the ability of hospital systems and first responders to screen and isolate potential Ebola patients.
With Ebola transmissions now documented in the U.S. and Europe — something that never happened before the current Ebola outbreak in Africa, which is the most widespread since the disease was first identified there in the 1976 — health officials worry about “loss of containment.” That worry is not just a concern about the spread of the disease itself, but also for the impact loss of containment will have on the ability of hospital systems and first responders to screen and isolate potential Ebola patients.
As it stands now, screening consists largely of asking patients with certain symptoms whether they’ve lived in or traveled to countries where the virus is active.
When questions about travel to West Africa are no longer relevant — in other words, if more Ebola diagnoses and transmissions are confirmed outside of West Africa — then local screening of patients presenting with known EVD symptoms becomes much more complicated and much more burdensome on local providers, PBMC’s Mitchell said.
“The early symptoms of Ebola are the same as the flu — fever, malaise, nausea, vomiting. If we can no longer rule out patients based on risk factors of travel to West Africa because the disease is active in Europe and the U.S., what happens when patients present with flu symptoms?” Mitchell asked. Flu season is just beginning, he noted. “The system will be quickly overwhelmed.”
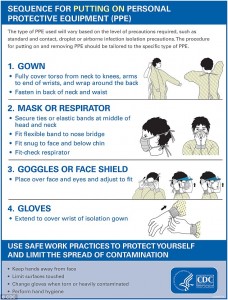 Under current CDC guidance, all health care workers handling symptomatic patients with risk factors for EVD must wear extensive protective gear and follow very specific rules for removing and disposing of the protective equipment. If the risk factors change — if containment is lost — following the same protocols for all patients with those flu-like systems will overload the system, Mitchell said.
Under current CDC guidance, all health care workers handling symptomatic patients with risk factors for EVD must wear extensive protective gear and follow very specific rules for removing and disposing of the protective equipment. If the risk factors change — if containment is lost — following the same protocols for all patients with those flu-like systems will overload the system, Mitchell said.
The prospect of every flu patient having to be ruled out by people wearing all that protective equipment is almost mind-boggling.
For one thing, Mitchell said, health care workers get burnt out. Wearing all that gear is uncomfortable. “It gets very warm,” he said. “Staff can only wear it for limited periods of time without a break. You have to rotate people out.” The process of safely removing the protective equipment is complex, difficult and time consuming, requiring a segregated area and a monitor to watch and oversee the process.
Then there’s the question of whether supply companies will be able to keep up with demand for the equipment. Tyvek suits are already backordered, Mitchell said.
“The probability of us getting a confirmed Ebola case is very low. The probability of us getting a suspected case is very high,” Mitchell said — even more so if the limiting risk factor of West African travel is no longer part of the screening equation.
“This is an especially important reason for everyone to get their flu shot this year,” Mitchell said. “You don’t want to contribute to the overload of the system and you don’t want to be put into a quarantine.”
Hospital ‘lockdown’ coming
 Beginning Monday, PBMC is essentially locking down its facilities, Mitchell said. There will only be three entrances to the hospital and staff will be posted at each entrance to screen all people entering the facility, asking questions about international travel and symptoms. The same procedures will be rolled out across PBMC’s health system, including walk-in clinics and doctors’ offices, Mitchell said.
Beginning Monday, PBMC is essentially locking down its facilities, Mitchell said. There will only be three entrances to the hospital and staff will be posted at each entrance to screen all people entering the facility, asking questions about international travel and symptoms. The same procedures will be rolled out across PBMC’s health system, including walk-in clinics and doctors’ offices, Mitchell said.
PBMC has been doing staff training for two months, but it is about to be stepped up. The hospital is putting together an Ebola management team, consisting of administrators, clinicians and bargaining unit representatives, Mitchell said. He’s arranged with North Shore/LIJ, where he worked before taking the helm in Riverhead in 2001, for PBMC to be included in staff training programs there. PBMC is sending a whole team to North Shore/LIJ’s training center next week, Mitchell said. That team will come back and train staff in Riverhead.
“Every hospital has to have the capability to care for a patient for a period of time until a patient can be ruled in or ruled out,” Mitchell said.
“We’re going to be doing a series of town meetings with the whole staff. Guidance is going to continue to change and we have to be adaptive,” Mitchell said. “We don’t want anyone to lose confidence because of the changes.”
The survival of local journalism depends on your support.
We are a small family-owned operation. You rely on us to stay informed, and we depend on you to make our work possible. Just a few dollars can help us continue to bring this important service to our community.
Support RiverheadLOCAL today.






























